Heat Injury and Illness Prevention
2025 OSHA Compliant Heat Injury and Illness Prevention Training Course

Course Overview: This comprehensive training is designed to fully comply with OSHA standards regarding heat-related illnesses. It addresses prevention, recognition, response, and reporting of heat-related conditions in the workplace.
Course Objectives:
- Understand OSHA's heat illness prevention guidelines
- Recognize the symptoms of heat-related illnesses
- Learn preventive measures and safe work practices
- Know how to respond in case of a heat-related emergency
Section 1: Introduction to Heat‑Related Illness
1.1 Overview of Workplace Heat Hazards
- Outdoor sun and radiant heat (e.g., roofing, paving). Workers laboring under direct sunlight or near hot surfaces such as asphalt or roofing materials absorb large amounts of radiant energy, which can dramatically raise skin and core temperature if not mitigated.

- Industrial equipment (furnaces, boilers, kilns). Hot-process machinery emits continuous heat; without insulation or shielding, employees working nearby may develop heat strain simply by proximity rather than physical exertion.
- Enclosed workspaces lacking adequate ventilation (attics, warehouses). When ambient heat has no outlet, air temperatures rise uncomfortably high, and humidity builds up—combining to overwhelm the body’s natural cooling mechanisms even at moderate activity levels.
1.2 Scope and Impact
- National statistics: Approximately 2,000 severe Heat Related Illness (HRI) cases and 30+ fatalities occur in U.S. workplaces each year. These figures, drawn from OSHA and CDC data, underline that heat illness remains a serious occupational threat rather than a rare anomaly.
- Economic burden: Medical treatment, lost workdays, increased insurance premiums, potential OSHA citations. Beyond human suffering, every case of HRI can lead to expensive hospital stays, costly workers’ compensation claims, and a tarnished safety record that invites regulatory fines.
1.3 OSHA’s Heat Illness Prevention Initiative
- “Water. Rest. Shade.” campaign emphasizes proactive controls. OSHA’s triad slogan reminds employers and employees alike that simple, low‑cost interventions—clean water, scheduled breaks, and shaded rest areas—form the foundation of any effective prevention plan.

- Compliance anchors: General Duty Clause (Section 5(a)(1)) and Sanitation Standard (29 CFR 1910.141). Under the General Duty Clause, employers must eliminate recognized hazards like heat stress, while the sanitation standard explicitly mandates sufficient potable water and cool rest facilities.
Section 2: Physiology of Heat Stress
2.1 Thermoregulation Basics
- Core vs. skin temperature; hypothalamus set‑point. The hypothalamus in the brain acts as a thermostat, striving to keep core temperature near 37 °C; skin temperature fluctuates more widely, reflecting environmental conditions and aiding heat exchange.
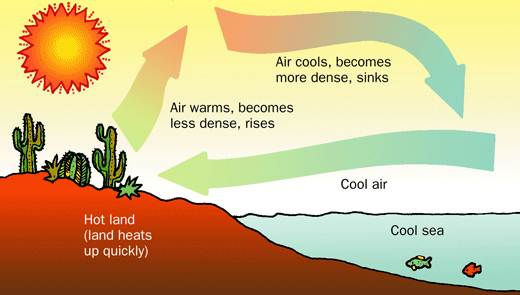
- Heat transfer pathways – conduction, convection, radiation, evaporation. Heat moves from hot to cold surfaces through conduction (direct contact), is carried away by moving air or water via convection, is emitted or absorbed as infrared radiation, and is dissipated when sweat evaporates off the skin’s surface.
2.2 Heat Index vs. Wet‑Bulb Globe Temperature (WBGT)
- Heat Index: Combines air temperature + relative humidity—useful for public advisories. When humidity is high, sweat cannot evaporate effectively, so the Heat Index gives a more realistic sense of “felt” temperature, but it ignores direct sunlight and wind.
- WBGT: Adds radiant heat and wet‑bulb measurements—preferred for occupational settings. By measuring black‑globe temperature (radiant heat) and wet‑bulb temperature (evaporative cooling potential) alongside air temperature, WBGT provides a comprehensive risk metric for planning work/rest schedules.
2.3 Individual Susceptibility Factors
- Non‑modifiable: Age (> 65), chronic illnesses. Older workers and those with conditions such as cardiovascular disease or diabetes have weakened thermoregulatory responses, so they require especially careful monitoring and accommodation.
- Modifiable: Hydration status, fitness level, acclimatization status. Well‑hydrated, physically fit, and gradually acclimatized workers tolerate heat far better; employers can promote these factors through policies and programs.
- Medications/Substances: Diuretics, antihistamines, stimulants, alcohol. Certain drugs reduce sweating or alter blood flow, while alcohol acts as a diuretic—each impairs the body’s ability to shed heat and increases HRI risk.
Section 3: Regulatory Requirements & Employer Obligations
3.1 Applicable OSHA Standards
- General Duty Clause obligates abatement of recognized hazards. Even without a specific “heat stress” standard, Section 5(a)(1) of the OSH Act requires employers to identify and correct serious heat hazards just as they would guard against machinery risks.
- 29 CFR 1910.141(b)(4): “Cool, clean, potable water must be readily accessible.” This sanitation rule ensures that workers can replace fluids lost through sweating, preventing dehydration and maintaining circulatory volume.

3.2 Heat Illness Prevention Plan Elements
- Roles & Responsibilities. Assigning clear duties—such as who reads WBGT devices, who approves rest breaks, who provides first aid—ensures no critical step is overlooked in the heat‑stress regimen.
- Environmental Monitoring. Placing calibrated WBGT monitors in representative work zones, with readings at least hourly when conditions warrant, lets supervisors adjust workloads in real time.
- Work/Rest Cycles. Defining specific on/off times based on WBGT thresholds (for example, a 20 min rest after 40 min of work at 88 °F WBGT) prevents overexertion during peak heat.
- Acclimatization Schedule. A phased plan (20% exposure Day 1, 40% Day 2, etc.) allows new or returning workers to build sweat‑response capacity without sudden overload.
3.3 Training Requirements
- Initial Training. Before any assignment in hot conditions, employees must learn HRI symptoms, hydration protocols, and how to use monitoring tools.
- Refresher Training. Annual updates reinforce best practices; “just‑in‑time” talks at the start of heat waves or new projects keep information fresh and context‑relevant.
- Content. Comprehensive curricula cover recognition of early and severe HRI symptoms, first‑aid steps for each condition, proper use of PPE, and hydration logging.
3.4 Employee Rights & Reporting
- Right to Stop Work. If a worker feels unwell from heat, they have protected leave to rest or seek shade without reprisal.
- Mandatory Reporting. Immediate notification to supervisors or safety officers when any HRI symptom appears ensures prompt intervention and prevents escalation.
Section 4: Recognizing & Responding to Heat‑Related Illnesses
4.1 Heat Rash
- Onset in humid conditions. When sweat ducts become clogged, trapped moisture causes red, itchy bumps especially under clothing or equipment straps.

- Treatment. Encouraging breaks in cool, dry areas and using talcum powder prevents secondary infection and relieves discomfort.
4.2 Heat Cramps
- Onset during/after exertion. Electrolyte loss and muscle fatigue trigger painful spasms in large muscle groups under sustained activity.

- First Aid. Resting in shade, gently stretching affected muscles, and sipping premixed electrolyte solutions restore salt balance and relieve pain.
4.3 Heat Exhaustion
- Core temp 100.4–104 °F. Fluid loss and circulatory strain produce heavy sweating, weakness, headache, and sometimes fainting if untreated.
- First Aid Steps.
- Move victim to shaded or air‑conditioned area.
- Loosen or remove excess clothing.
- Apply cool, damp cloths to neck, groin, and armpits.
- Offer small, frequent sips of cool water or electrolyte drink while monitoring for improvement.
- Move victim to shaded or air‑conditioned area.

4.4 Heat Stroke
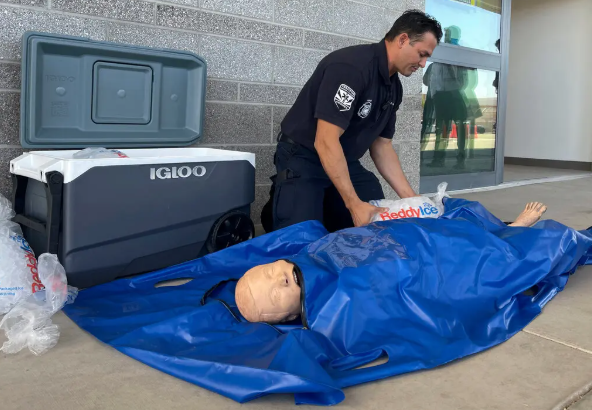
- Core temp ≥ 104 °F with CNS impairment. The brain overheats, leading to confusion, seizures, or loss of consciousness; sweating may paradoxically cease.
- Emergency Protocol.
- Call 911 without delay.
- Begin rapid cooling via ice‑water immersion or ice packs on major arteries (groin, neck, armpits).
- Continually monitor airway, breathing, and pulse until EMS arrives.
- Call 911 without delay.
Section 5: Prevention Strategies
5.1 Engineering Controls
- Ventilation & climate control. Installing exhaust fans, evaporative coolers, or air‑conditioning removes heat before it impacts workers directly.
- Barriers & insulation. Wrapping hot pipes, erecting reflective shields, and insulating furnaces minimize radiant heat in work zones.

- Spot Cooling. Portable fans or misting units directed at individual workstations provide immediate relief at low cost.

5.2 Administrative Controls
- Scheduling. Shifting heavy tasks to early morning or evening hours when ambient temperatures are lower reduces peak heat exposure.

- Work/Rest Cycles. Tailoring work and break durations to real‑time WBGT readings prevents cumulative heat strain throughout the shift.
- Acclimatization Program. A staggered approach over 5–7 days lets physiological adaptations—like increased sweat rate and stabilized circulation—develop safely.
5.3 Hydration Protocols
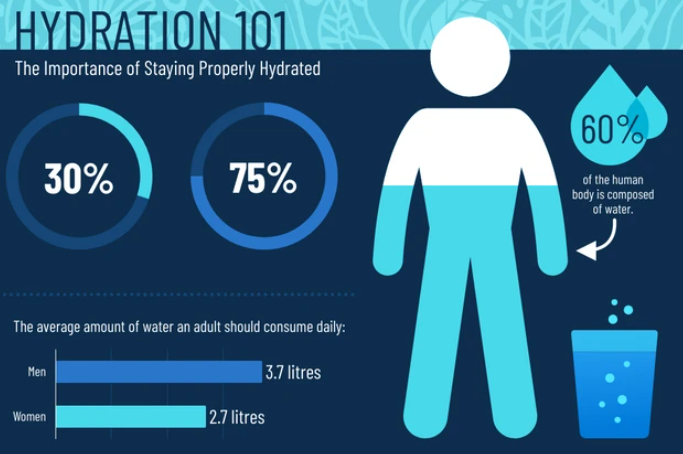
- Water access. Providing cool, potable water within 25 ft of work areas and encouraging at least one cup every 15 min keeps blood volume stable.
- Electrolyte solutions. Offering balanced salts and sugar in oral rehydration mixes replaces sodium and glucose lost through sweating.
- Hydration monitoring. Logging individual fluid intake helps identify workers lagging in consumption before symptoms appear.
5.4 Personal Protective Equipment (PPE)

- Breathable clothing. Light‑colored, moisture‑wicking fabrics allow sweat evaporation while reflecting solar radiation.
- Cooling accessories. Evaporative vests and soaked neck wraps draw heat away from the trunk and major blood vessels.

- Headgear. Ventilated hard hats or cooling caps protect against direct sun and trap sweat for gradual cooling.
Section 6: Emergency Response & First Aid
6.1 Emergency Action Plan Components
- Activation protocols. Alarms, two‑way radios, or phone trees mobilize first‑aid responders within seconds of a suspected HRI event.

- Roles & responsibilities. Pre‑assigned responders know exactly which supplies to grab and how to reach medical services quickly.
- Equipment locations. Clearly marked heat‑stroke kits—complete with ice packs, thermometers, and oral rehydration salts—must be within a minute’s reach.

6.2 First‑Aid Protocols by HRI Stage
- Heat Rash: Monitor for secondary infection; no hospital treatment needed unless rash spreads or worsens.
- Heat Cramps: After relief, resume light activity only with adequate hydration; seek medical evaluation if cramps recur.
- Heat Exhaustion: If symptoms persist beyond 30 minutes of cooling and fluids, arrange medical transport.
- Heat Stroke: Never delay: even a few minutes of elevated core temperature can cause irreversible organ damage.
6.3 Post‑Incident Procedures
- Medical clearance. Require a health‑care provider’s written authorization before returning the affected employee to heat duties.
- Incident investigation. Collect WBGT logs, interview witnesses, and pinpoint failures (e.g., missed breaks, inadequate shade).
- Corrective actions. Update the prevention plan, retrain staff on any gaps discovered, and improve controls to prevent recurrence.
Section 7: Training Delivery & Documentation
7.1 Effective Training Methods
- Toolbox talks. Brief, focused discussions at the start of shifts keep the topic fresh and relevant to that day’s conditions.

- Hands‑on drills. Practicing WBGT measurement, PPE donning, and first‑aid drills builds muscle memory for rapid response.

- Multimedia aids. Short videos demonstrating early symptom recognition, followed by guided Q&A, reinforce learning for diverse audiences.
7.2 Recordkeeping Best Practices
- Training logs. Track attendance, quiz scores, and topics covered; retain records for at least three years per OSHA guidelines. Note: This is all accomplished through BloodBornePathogensTrainingOnline.com.
- Incident reports. Document date/time, environmental readings, response actions, and medical follow‑up to facilitate trends analysis.
- Equipment maintenance. Record calibration dates for thermometers and WBGT gauges to ensure accuracy.
7.3 Continuous Improvement
- Program reviews. After each heat wave or HRI event, convene safety teams to assess what worked and what needs strengthening.

- Worker feedback. Use anonymous surveys or suggestion boxes to gather frontline insights on plan feasibility and comfort.
- Plan updates. Revise written procedures, adjust schedules, or add controls based on real‑world performance and evolving best practices.
End of Training Section.
Congratulations! You have completed the OSHA Heat Related Illness Training Section.
You may now proceed to Testing.
Testimonials
Individual
"Thanks for the fast service! I needed my certification before I could begin my new job. I was able to complete the test and print my certificate in time to start work Monday morning." Janet F., Orlando, FL.
Company
"Over 200 employees throughout our offices are required to complete Blood borne Pathogen Certification annually. Employee availability and scheduling conflicts made it nearly impossible to schedule an onsite class. We were pleased to learn that our OSHA requirements can be satisfied online. Looking forward to the ease of use next year." Mary M., Cardinal Health
Follow Us
Contact Us
Have a question? Customer service representatives are standing by to assist.

